On this page:
Introduction
We are here to help people with work-related injuries or illnesses receive the health care they need to recover and return to work. Through the programs of care, we work with community health care providers to facilitate access to the delivery of evidence-based health care for specific illnesses and injuries.
The musculoskeletal (MSK) program of care is a community health care program providing evidence-based care for musculoskeletal injuries. We developed the program with input and recommendations of a working group made up of regulated health professional representatives with the relevant qualifications and clinical experience. The professions who participated are those most involved in the delivery of the WSIB programs of care. Key goals in the development of this program were streamlining access to care and reducing administrative burden in the delivery of the program for injured people and health care providers. This revised program launched in April 2023.
All regulated health professionals whose scope of practice, knowledge and skill include the assessment, treatment and rehabilitation of musculoskeletal injuries may deliver the musculoskeletal program of care. This includes the ability to deliver all interventions, either as a sole provider or as part of an interdisciplinary team.
Regulated health professionals must register with the WSIB to deliver the musculoskeletal program of care. Providers who are already registered to deliver programs of care must re-register. A diagnosis is required to guide the person’s treatment plan. This diagnosis is provided by a regulated health professional who is a WSIB primary provider (physician, physiotherapist, chiropractor, nurse practitioner). Other regulated health professionals may deliver the musculoskeletal program of care if it is within their scope of practice, they have met all registration requirements and they have received a referral from a WSIB primary provider.
The musculoskeletal program of care does not replace regulatory college requirements (e.g., consent, documentation) of the regulated health professional in practice or the professional judgement of the treating regulated health professional.
We will evaluate the musculoskeletal program of care following implementation to continuously monitor the quality of services, including recovery and return-to-work outcomes.
Program objectives
The objectives of the musculoskeletal program of care include:
- facilitating timely access to evidence-informed, individualized musculoskeletal assessment and treatment
- facilitating recovery of overall function with specific focus on safe, timely and sustained return to occupational function
- identifying and monitoring functional abilities and restrictions for return-to-work planning
- preventing ongoing/prolonged symptoms
- identifying people who are not responding to the musculoskeletal program of care treatment and recommending appropriate assessment and intervention
- providing detailed information that supports people’s recovery and return to work
- improving communication and satisfaction among people with musculoskeletal injuries, health care providers, employers, WSIB and other stakeholders
Admission criteria
The musculoskeletal program of care is for people who:
- have a pending or allowed WSIB claim for a single zone of injury, or
- have an allowed WSIB claim for multiple zones of injury
- are within eight weeks from their date of workplace injury
- have an injury to:
- a muscle, tendon, ligament, fascia, intra-articular structure or any combination of these structures, causing mild to moderate damage (Grade I or Grade II) and/or
- a bone, resulting in fracture(s) that did not require surgical intervention
- are at work or off work
- have no additional injuries that prevent participation in this program of care
- are not hospitalized
We do not recommend the musculoskeletal program of care for people who are not medically cleared to begin rehabilitation or who have contraindications to receiving treatment in this program.
If the injured person is not within the admission criteria, or if you have any questions about eligibility, please contact the Clinical Expert Line at 416-344-5739 or toll free 1-866-716-1299 Monday to Friday from 7:30 a.m. to 5 p.m.
Single zone of injury versus multiple zones of injury
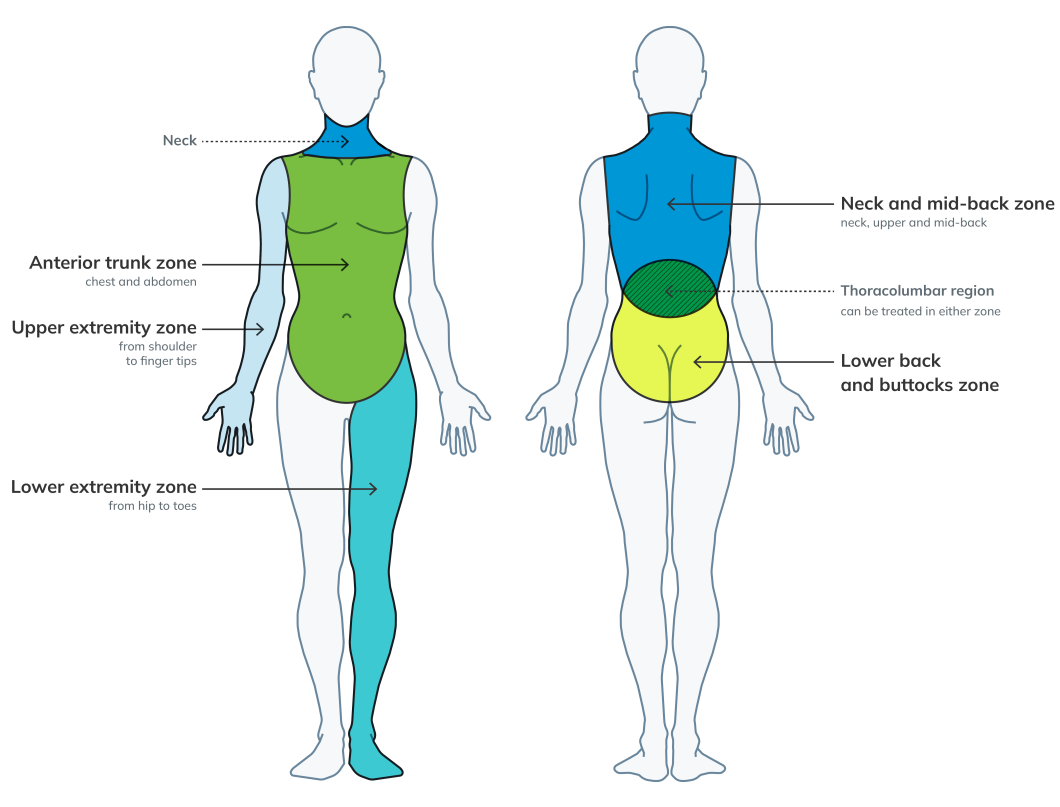
A single zone of injury is defined as any or all injuries in one anatomical zone, while multiple zones of injury is defined as any or all injuries in two or more anatomical zones.
There are five distinct anatomical zones.
Using the diagram for reference, an injured person with a left shoulder sprain/strain and a left wrist sprain/strain would be considered as having a single zone of injury – the left upper extremity zone. If the person has an injury to the left knee and the lower back, these injuries would constitute multiple zones of injury, namely the left lower extremity zone and the lower back and buttocks zone.
Any injuries to structures of the pectoral or pelvic girdles are treated within the corresponding upper or lower extremity zone. Overlap between the neck, upper and mid back zone and the lower back and buttocks zone is considered to allow for injuries to the thoracolumbar region, which can then be treated in either one of these zones.
If you are providing treatment that is limited to monitoring or advising for a minor injury (i.e., bruise, cut), in addition to the primary zone of injury, this injury would not be considered as a separate zone of injury. In addition, in cases where the mild traumatic brain injury (mTBI) program of care is being delivered, treatment of the neck is included in the mild traumatic brain injury program of care and will not be considered as a single zone of injury within the musculoskeletal program of care.
Single zone of injury
Where there is a single zone of injury, to enable early access to care, you can deliver block one treatment of the musculoskeletal program of care regardless of if the registered claim is pending or allowed. You must confirm entitlement prior to delivering block two treatment.
Multiple zones of injury
If a person has multiple zones of injury, call us to confirm approval for the treatment of multiple zones of injury at the beginning of block one. You may begin the musculoskeletal program of care if approval is still pending, but we would only pay you for block one for a single zone of injury if approval is not later granted for multiple zones of injury. If we authorize care for multiple zones of injury, you receive an increased fee.
Assessment of risk factors
Some people may have risk factors that could indicate the need for urgent care or specialized services. You may identify risk factors during the initial assessment or during the course of treatment. As soon as you identify any risk factors, you must immediately call our Clinical Expert Line to discuss possible referral to specialized services.
These risk factors may include:
- significant neurological deficits (e.g., major motor weakness, disturbance of bowel or bladder control)
- signs of infection, tumour, pathological fractures or a systemic condition
- worsening of symptoms or increasing number of symptoms
- other risk factors not otherwise listed
Program structure and duration
The musculoskeletal program of care is up to eight weeks in length and consists of two blocks of care. The first block includes the initial assessment and four weeks of treatment. The second block comprises four weeks of treatment.
Initial assessment and report
Before starting treatment, the treating regulated health professional conducts an assessment. The components of the initial assessment must conform to the professional guidelines and standards of practice within each regulated health profession, and within the framework of evidence-informed practice for the treatment of musculoskeletal injuries. The length of a typical initial assessment for people with a musculoskeletal injury will vary for each individual, and may take longer than the initial visit.
The assessment should include the following key elements:
- medical history including the identification of pre-existing conditions that may impact the person’s recovery
- identification of their specific musculoskeletal symptoms
- summary of the physical findings including the testing completed
- screen for risk and other barriers to recovery and return to work
- administration of outcomes measures for baseline scores related to symptoms and function
- establishment of the person’s functional abilities with respect to activities of daily living and/or work
- determination of the person's current abilities and restrictions for return-to-work planning
- development of a treatment plan
Musculoskeletal initial assessment report
Treatment and reporting
Block one
- Call us at the end of block one if the person’s entitlement status is still unknown
- Call our Clinical Expert Line at the end of block one if you identify a lack of progress in functional abilities or more than two barriers
Block two
- Call our Clinical Expert line one week before completing block two if you do not expect the person to make a full recovery and/or return to work, and you are recommending additional treatment.
You can discharge the person and submit the care and outcomes summary at any time if their recovery and return-to-work goals have been met.
If the person is not progressing as expected at any time during the program, call us to discuss options for specialized assessment.
The recommended evidence-informed interventions
The musculoskeletal program of care is based on the principles of evidence-based medicine, defined as “the conscientious, explicit and judicious use of current best evidence” (Sackett et al. 1996), in making decisions about the care of people with injuries. We previously conducted systematic reviews of the scientific literature in the development of the original musculoskeletal-focused programs of care. Although the body of research may have grown, the approach to the treatment of musculoskeletal injuries has remained largely consistent since these reviews.
The treating regulated health professional should chose treatment interventions based on their clinical judgement and take into consideration the person’s functional recovery needs. As a sole provider or part of an interdisciplinary team, you must be able to deliver all interventions in order to deliver the musculoskeletal program of care. The following interventions are recognized as evidence-based treatment interventions typical for the treatment of a wide variety of musculoskeletal injuries suitable for this musculoskeletal program of care.
You should use the following treatment interventions in the most effective combination, frequency and intensity based on clinical judgement, the clinical findings and on the person's functional needs.
Education
Education is a required intervention for people in the musculoskeletal program of care. Regardless of the time of entry into the program, the person’s first treatment should consist of education about musculoskeletal injuries and self-management strategies for symptoms related to their musculoskeletal injury.
Education provides people with the context to better understand their condition and the expected treatment outcomes. Education should be ongoing and embedded within every intervention with them to maximize its benefit.
Education should include:
- an explanation of the injury (in anatomical and physiological terms understandable to the individual)
- explanation about the typical timeframes and pattern of recovery
- review of the treatment and recovery plan
- discussion about the importance of early activity and stay at work or return to work
- education about the gradual reintegration of appropriate physical activities, activities of daily living, and homework activities
- identification and discussion about risk factors / flags noted
- engaging the person in their own recovery
- better at work principles and
- appropriate adult education methods (i.e., verbal and written), including an opportunity to ask questions
Pain and self-management strategies
You should share pain and self-management strategies with the person in the program.
These may include strategies such as:
- changing posture after a given period of time
- applying ice to an injury
- promoting self-mobilization and progression of activity at home and at work
- recommending against prolonged or total rest
- emphasizing recovery and restoration of function
- encouraging participation in exercise with gradual increase in usual activity and occupational tasks
Where pain is a focus, education has an even greater importance. For people experiencing pain, education should include techniques for coping with persistent symptoms such as sleep hygiene, stress management and pacing and planning activities.
Activity modification
You should also discuss education around activity modification with the person, such as recommendations on how to use the injured area in daily activities. Appropriate activity modification emphasizes the temporary nature of any restriction and highlights activities that are safe to complete.
Graded activity is a progressive increase in activities from the baseline toward predetermined goals within a defined period of time. It often helps to reduce pain, disability and absence from work more effectively than other treatment interventions. In some cases, you may suggest simple environmental modifications such as arranging a workspace to reduce strain on an area of injury to facilitate recovery and return to work. It is important to note that environmental modifications requiring devices or equipment are not within the scope of this program. If recommended, please call us.
Exercise therapy
Rehabilitation of muscles, tendons and ligaments should focus on restoring range of motion and strength using functional exercises as early as possible and culminating in task-focused rehabilitation.
Exercises are more effective when tailored to the individual and to functional requirements. Complex exercises, often referred to as motor-learning, neuro-muscular re-educating, functional exercises, coordination exercises, stabilization programs and proprioceptive re-training, help to restore normal activity, movement and function. You should supervise the exercise program and reinforce it with a home exercise program. Exercise should be progressive, with increasing intensity, as the person recovers and improves.
Manual therapy
Manual therapy includes many forms of hands-on therapy such as joint manipulation, joint mobilization, passive and assisted range of motion, manual traction and various soft tissue treatment modalities including massage therapy, myofascial release techniques, etc. You can use one or multiple forms of manual therapy to treat an injury.
In general, manual therapy may aid recovery by helping to manage pain, reduce swelling, improve range of motion, improve flexibility and mobility, and promote relaxation.
Adjunct therapeutic interventions or modalities
In some cases, you can include adjunct therapeutic interventions or modalities (i.e., ice, heat, electrotherapy modalities, acupuncture, laser therapy, ultrasound, shockwave therapy, etc.) for pain reduction as part of the overall rehabilitation program. These therapeutic interventions or modalities should not be the sole treatment intervention delivered. For those injuries where their use is considered, you should support their delivery by best evidence and clinical need.
Some injuries to the extremities may require temporary immobilization using a removable brace, cast or splint. The benefits of temporary immobilization include maintaining activity and usual functioning while protecting the injured site.
Goal setting or treatment planning
When completing the initial assessment and mid-point reports, the regulated health professional and the person will identify recovery and return-to-work goals to support occupational functional recovery.
Goal setting helps direct rehabilitation interventions toward patient-centered outcomes and can result in greater patient satisfaction and improve recovery. It can also help you plan your interventions. A meaningful goal can increase the person’s engagement and motivate them to participate in functional recovery. Additionally, you can use treatment goals to evaluate the success of rehabilitation interventions.
Within the context of rehabilitation, there is a body of literature that is dedicated toward guiding principles, theories and methods for goal setting. One common standardized method of defining goals in rehabilitation settings is the SMART method.
There are some variations, but the generally accepted SMART acronym stands for:
- Specific – clear description of the desired outcome
- Measurable – includes a method of measuring achievement of the goal (e.g., numbers, quantities, repetitions, etc.)
- Attainable/achievable – the goal is reasonable to achieve
- Relevant/realistic – it is applicable to functional recovery and return-to-work activities
- Time-bound – includes a clear timeline to achieve the goal
- An example of a SMART goal is the injured person will be able to lift a 30lb box from the floor to waist level using both hands within six weeks.
Return-to-work planning
As a health care provider, you play an important role in planning for early, safe and sustainable return to work. The information you gather during the initial assessment, mid-point, and care and outcomes summary report will support the process. In the musculoskeletal program of care, we expect you to document detailed functional abilities information.
In each of the musculoskeletal program of care reports, the final page includes a section for abilities and restrictions for return-to-work planning. You will need to document the injured person’s abilities, limitations, restrictions and accommodations. This information will support return-to-work planning, as it will specify/highlight what the person can do in each phase of recovery, including limitations and appropriate accommodations.
With detailed information about the person’s abilities, we can identify suitable work as they continue to recover. If the person shares a job description or letter of modified work with you, you can use this information to complete this section of the report.
Once you complete the abilities and restrictions for return-to-work planning page on the report, you can give the patient a copy for their own information and to share with their employer. We will receive a completed copy when you submit the report through our online services.
Barriers to recovery
During the initial assessment and treatment, you will need to identify any barriers to recovery and return to work. Early identification of barriers is important as early intervention can help to reduce chronicity and support recovery and return-to-work goals.
Barriers that may impact someone’s functional recovery or improvement include:
- Fear/avoidance of activity
- Co-morbid conditions
- Limited support
- Believes hurt equals harm
- Low mood/social withdrawal
- Does not feel ready for return to work
- Medium to heavy job duties
- Working conditions and/or shift work
- Difficulty transitioning from modified to pre-injury duties
- Does not feel current work duties are suitable
If the individual displays any barriers that may impact functional recovery or interferes with the successful participation in the musculoskeletal program of care, you should identify the relevant factors in the musculoskeletal program of care reports and include any supporting details in the section.
Outcome measures
Outcome measures are validated tools that measure function and disability, which can help health care providers and our Case Managers understand the impact of musculoskeletal injuries over time. Outcome measures can also help measure a person’s clinical and functional progress or improvement.
There are five functional outcome measures used in the musculoskeletal program of care.
Neck
-
The(NDI) is a 10-item questionnaire used to measure self-rated disability due to neck pain.
Lower back
-
The(also known as the Oswestry Disability Index, ODI) is a 10-item questionnaire that assesses how a patient’s back pain or leg pain has affected one’s ability to manage everyday life.
Upper extremity
-
Theis a shortened version of the Disabilities of the Arm, Shoulder and Hand (DASH) outcome measure used to evaluate physical function and symptoms in patients with musculoskeletal disorders of the upper extremity. In addition to the 11-item questionnaire, providers are expected to also complete the “Work Module” component.
Lower extremity
-
-is a 20-item questionnaire used to measure a person's ability to perform everyday tasks in patients with musculoskeletal conditions affecting the lower extremity.
Generic musculoskeletal
-
is a generic assessment instrument for health and disability. It covers six domains of functioning including: cognition, mobility, self-care, interacting with people, life activities (home, work, school, leisure) and participation in community activities.
At the initial assessment, you will need to select the most appropriate outcome measure to administer from the list of functional outcome measures. You may administer more than one functional outcome measure in cases of multiple musculoskeletal injuries (i.e., a low-back injury and a right-knee injury). Repeat the outcome measures selected at initial assessment at the time of the care and outcomes summary report.
You may use additional outcome measures not listed, as appropriate.
Staying at or returning to work
Staying at work or returning to work at the right time is important in a person's progress toward functional recovery and a successful and sustained return to work.
There is evidence that staying at work or returning to work following injury enhances recovery, general health and long-term employment outcomes. See our Better at Work principle. Research shows that people with injuries or illnesses heal faster and avoid or reduce permanent physical or psychological impairments by integrating health care with return to suitable and safe work.
Full recovery is not a requirement for return to work. In most cases, returning to work will require a phased approach based on the person’s recovery and type of employment. Your role when delivering the musculoskeletal program of care is to identify the patient’s abilities, limitations and required accommodations to help inform return-to-work opportunities.
Additional treatment: supplementary block
Sometimes, the person may need additional treatment through the musculoskeletal program of care to meet their recovery and return-to-work goals.
In these instances, once approved, you can use a four-week supplementary block of treatment. You will need to call our Clinical Expert Line to discuss the rationale for additional treatment including discussing current clinical and functional information, changes in outcome measures, barriers to recovery, treatment frequency/duration and overall recovery and return-to-work goals. It is expected that treatment is delivered as often as necessary within the block to achieve recovery and return-to-work goals, with a minimum of three sessions.
You must submit a supplementary report at the end of the supplementary block.
If the person needs more than one supplementary block, the WSIB must approve each supplementary block.
After a specialized assessment completed by WSIB contracted providers, continued community treatment through the musculoskeletal program of care delivered through supplementary blocks may also be recommended.
Communication and reporting
Timely and effective communication with the WSIB is an important element in the success of the musculoskeletal program of care. Communication includes written reports, telephone conversations and one-on-one discussions. The frequency of communication varies depending on individual circumstances and the extent of progress achieved.
When should I call with the WSIB?
You must call the WSIB in the following scenarios:
- At the beginning of block one to confirm entitlement to multiple zones of injury
- At the end of block one to confirm entitlement for a single zone of injury, if unknown,
Call the Clinical Expert Line if:
- The injured person does not meet the admission criteria for the musculoskeletal program of care
- At the end of block one if you identify a lack of progress in functional abilities or more than two barriers to recovery
- The injured person is not expected to meet their recovery and return-to-work goals one week before completing the second block
- There are delays or interruptions (e.g., illness) in services that lasts beyond one week
- If the person’s recovery is not progressing as expected at any time during the program to discuss options for specialized assessment/treatment.
Call the Case Manager or Nurse Consultant if:
- Additional treatment is required after the first supplementary block
- The person’s recovery is not progressing as expected at any time during the program
- You are looking for more information related to return to work or employer accommodations to help with your treatment planning
You should also communicate with the person’s family physician, or other treating health care providers.
Reporting required during the musculoskeletal program of care include:
- – submit two business days after completing the initial assessment
- – submit two business days after last treatment session in block one
- – submitted two business days after discharge. You must call us:
In the musculoskeletal program of care reports, once the abilities and restrictions for return-to-work planning page is completed, you must give a copy to the person to share it with their employer. We will receive a completed copy when the report is submitted through our online services.
Additional referral recommendations
In some cases, a person may benefit from additional referral for assessment or intervention. If recommended, we will help to facilitate access to our continuum of care, including expedited access to musculoskeletal assessment and other treatment available, including physician specialists, surgery and interdisciplinary care. You can recommend this to us by it your reports and by calling us.
Resources
For general inquiries, call 1-800-387-0750.
Clinical Expert Line
To reach our Clinical Expert Line, please call 416-344-5739 or toll free 1-866-716-1299 Monday to Friday from 7:30 a.m. to 5 p.m.
Provider registration
To report any changes to your listing in the musculoskeletal program of care directory, email [email protected] or call us at 416-344-4526 or 1-800-569-7919.
Submit musculoskeletal program of care reports online
Providers can submit all musculoskeletal program of care forms through our online services. You will need to create an online services login or account to submit documents. If you have questions or trouble submitting a document, call 1-800-387-0750, Monday to Friday from 7:30 a.m. to 5 p.m.
Billing and payment
In the musculoskeletal program of care, regulated health professionals must submit bills electronically through our online services on the TELUS Health Provider Portal. For help with electronic billing, please contact the TELUS Health Solutions at 1-866-240-7492 or visit telushealth.com/wsib
For more information on health care payments, please call us at 1-800-387-0750 or 416-344-1000.
Acknowledgements
The following regulated health professional associations made significant contributions to the development of the musculoskeletal program of care.
- Ontario Chiropractic Association
- Ontario Physiotherapy Association
- Ontario Society of Occupational Therapists
- Ontario Kinesiology Association
We appreciate their participation.
References
Sackett et al. (1996). Evidence based medicine: what it is and what it isn’t. BMJ, 312, 71-72.
Updated: