Program overview
Is the musculoskeletal program of care the mandatory first line of care, similar to the mild traumatic brain injury program of care?
Yes, the musculoskeletal program of care is the mandatory first line of care for musculoskeletal injuries. It is an evidence-based health care delivery program that aims to achieve the best recovery and return-to-work outcomes for people with a musculoskeletal workplace injury.
The musculoskeletal program of care allows early access to care, focuses on function and enables quick identification of cases that need specialized services. Reports for the musculoskeletal program of care provide us with detailed information that supports people’s recovery and return to work.
How does the Clinical Expert Line support regulated health care providers delivering programs of care?
The Clinical Expert Line is a WSIB phone line that health care providers can call to ask questions about specific claims. Our clinical experts are regulated health professionals who have peer-to-peer clinical conversations with regulated health professionals providing care to injured people about aspects of a claim such as diagnosis, treatment and barriers to recovery.
Our clinical experts help health care providers determine the suitability of a program of care for the injured person they are treating, discuss next steps when someone’s response to treatment is not progressing as expected and approve a supplementary block of treatment, if required.
To reach the Clinical Expert Line, please call 416-344-5739 or toll free 1-866-716-1299 Monday to Friday from 7:30 a.m. to 5 p.m.
Can I deliver the musculoskeletal program of care virtually?
You must deliver the musculoskeletal program of care in person, unless there is an exceptional circumstance justifying virtual care, which would need to be approved by the WSIB.
Do I need to register to deliver the musculoskeletal program of care?
Yes, you will need to register to be able to deliver the musculoskeletal program of care. This will allow your contact information to be posted on a new directory, to assist injured people in finding care quickly and close to home. You will be required to review all program resources as part of your online registration.
Will you monitor and measure care delivered through the musculoskeletal program of care?
Yes, the WSIB will evaluate quality and outcomes to allow for continuous improvement. This information will be shared with health care professional associations that deliver care through the musculoskeletal program of care.
Program eligibility and admission requirements
How should regulated health professionals proceed if they assess someone and determine that they do not meet the musculoskeletal program of care admission requirements?
You should call our Clinical Expert Line to discuss the case and determine the best way to proceed. Our clinical expert may suggest referral for specialized services or further assessment to determine what care is required. There may also be cases where someone doesn’t meet admission criteria, but the musculoskeletal program of care is still appropriate for delivering treatment.
To reach our Clinical Expert Line, please call 416-344-5739 or toll free 1-866-716-1299 Monday to Friday from 7:30 a.m. to 5 p.m.
How does the musculoskeletal program of care define injuries?
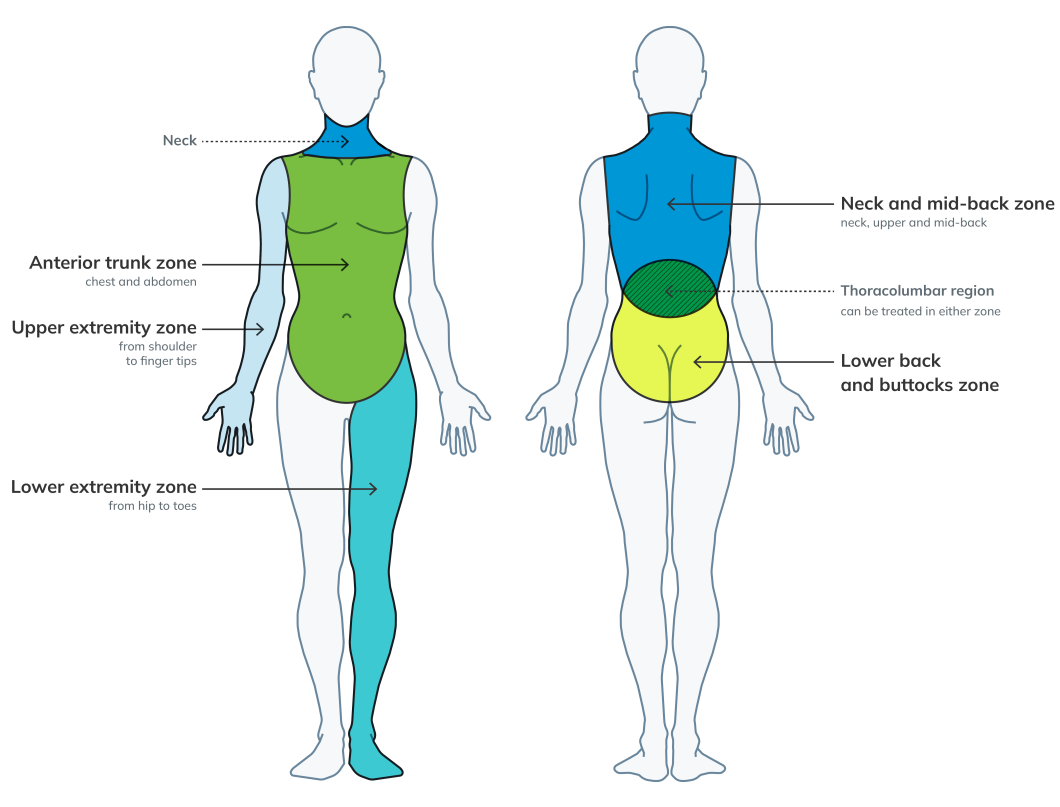
A single zone of injury is defined as any and all injuries in one anatomical zone, while multiple zones of injury is defined as any and all injuries in two or more anatomical zones.
Examples of single zone and multiple zones of injury:
- Example one: If the injured person has a left shoulder sprain/strain and a left wrist sprain/strain, these injuries would fall under a single zone of injury – the left upper extremity zone.
- Example two: If the injured person has an injury to the left knee and the lower back, these injuries would fall into two zones (which is considered multiple zones) - the left lower extremity zone and the lower back zone.
- Example three: If the injured person has a left shoulder injury and a right shoulder injury, i.e., a bilateral shoulder injury – these would fall under the multiple zone category.
- Example four: If an injured person has a thoracolumbar injury, the provider would decide whether to treat the thoracolumbar injury as either part of the mid-back zone, or part of the lower-back zone – since the thoracolumbar region is a transitional zone. The thoracolumbar injury would fall under a single zone of injury.
If someone’s claim is pending, can I deliver treatment in the musculoskeletal program of care?
Single zone of injury
- To enable early access to care, if a person has a single zone of injury, you can deliver block one treatment of the musculoskeletal program of care, whether the claim is pending or approved. If their claim is pending, you must confirm the claim is approved before you start delivering block two treatment.
Multiple zones of injury
- If a person has multiple zones of injury, you must get approval from the WSIB to begin treatment to more than one zone before delivering block one. You can begin treating multiple zones of injury without WSIB approval but are only paid for block one single zone of injury if approval is not granted for multiple zones of injury. Providers receive increased fees when care is authorized for multiple zones of injury.
If we approve a single zone of injury in block one, or you have received approval to treat multiple zones of injury in block one, please continue treatment into block two. You do not need to call us in this case.
How do I know if a claim is registered, pending or allowed?
Following a work-related injury, the injured person and their employer must report the injury to us. Once they’ve reported the injury, we will register the claim and send a claim number to the person with the injury. Receiving a claim number does not mean the claim is approved.
The registered claim is “pending” until we make a decision to accept the work-related injury or illness and approve health care benefits.
When someone seeks treatment, during the assessment you should ask whether the injury is work related and if they have registered a claim with the WSIB. If they have, ask for the claim number and status.
At any time, if their claim status is uncertain, you or your patient can call us at 1-800-387-0750 or 416-344-1000 to check the status of the claim.
Should a health care provider complete a Form 8 and the new musculoskeletal program of care initial assessment report?
Only physicians, physiotherapists, chiropractors and nurse practitioners are authorized to complete a Form 8.
If you are authorized to do so, you should complete both the Form 8 and the initial assessment report if you are the first regulated health care providers to assess a person following an injury.
Can someone switch from a single zone of injury to multiple zones of injury if they started treatment in a single zone category?
Yes. If you identify an additional zone of injury during treatment, call the WSIB for approval to treat multiple zones of injury. When approved, you can begin to deliver care to multiple zones and bill the increased fee for the current block of treatment.
When would additional musculoskeletal treatment services be allowed at the same time as the program of care?
This musculoskeletal program of care is a first line bundled program where the regulated health care professional may deliver as many treatment interventions as needed (based on their clinical judgment) as a sole provider or as part of an interdisciplinary team. Payment for all treatment services rendered are included in the musculoskeletal program of care block fee.
If a person’s musculoskeletal injury falls outside of the admission criteria, or there are multiple zones of injury, call the Clinical Expert Line to ensure that the musculoskeletal program of care is the appropriate level of care or if more specialized care is required.
Registration
On the musculoskeletal program of care provider registration form, there is a field for 'Provider billing ID number'. Should I enter my individual provider ID or the clinic provider ID?
The provider ID you enter determines where we will direct payment. To direct the payment to you, enter your individual provider ID number. To direct the payment to the clinic you work at, enter the clinic provider ID. In this scenario, the clinic is responsible for making the necessary disbursement of payment to their interdisciplinary team members involved in the delivery of care.
If a regulated health professional works in multiple clinics, they must register each location. Does this mean they need to have a different provider ID for each clinic they work at?
The provider ID you enter determines where we will direct payment. If you work at multiple clinics, and we are sending payment to the clinic, you must enter each clinic’s provider ID on each respective registration form.
If a provider enters their individual provider ID, can they still opt to bill under the clinic's provider ID if they want to direct the payment to the clinic?
Yes, you can use the clinic’s provider ID to bill for services delivered by any regulated health care professional working at the clinic, once they are registered.
Program delivery and structure
Who can deliver the musculoskeletal program of care? When is a referral required?
Regulated health professionals may deliver the musculoskeletal program of care if it is within their scope of practice and their individual knowledge, skill and judgement. Given the requirement for providing a diagnosis, where the regulated health professional is not a WSIB primary provider (chiropractor, physiotherapist, physician, nurse practitioner), they may still deliver the program provided it is within their scope of practice, they have completed their registration with us and have received a referral from one of the WSIB primary providers. Any regulated health professional who receives a referral from a primary provider is expected to maintain communication with the primary provider to discuss any change in status.
What is required to register to deliver the musculoskeletal program of care?
Providers interested in delivering the musculoskeletal program of care must register with us online.
To deliver the program, regulated health care professionals must complete the following steps:
- Review all program materials on our website, including the musculoskeletal program of care reference guide, outcome measures, forms/reports, fee schedule and training slides. If you attended the training webinar, the recordings are available through your association. If you did not attend a training webinar with an association, please review the training slides on our website.
- Get an electronic billing number and a WSIB Provider ID number by registering with TELUS Health.
- Sign up for an online services account with us, if you do not already have one, to submit program of care forms.
- Complete the musculoskeletal program of care registration form.
You will be registered as an individual, not as a clinic, therefore every regulated health professional wanting to deliver this program must be registered, even if delivering the program as part of an interdisciplinary team. Even if you are currently registered to deliver a program of care you must reregister specifically for the musculoskeletal program of care.
What happens if I choose to not deliver the musculoskeletal program of care?
If you choose to not treat an eligible injured person through the musculoskeletal program of care, you must refer the injured person to another regulated health professional who will deliver the musculoskeletal program of care. You can call us for help finding regulated health professionals who deliver the musculoskeletal program of care by geographic area.
What is the length of the musculoskeletal program of care and how many visits must a provider complete?
The length of the musculoskeletal program of care is up to eight weeks in duration. It is expected that you treat the injured person as often as is necessary to achieve their recovery and return-to-work goals. A minimum of five visits is required in block one, four visits in block two and three visits in the supplementary block (if approved) to bill the full program fee. If the minimum visits are not delivered, you will be paid 50 per cent of the applicable block fee.
How is the first date of service/treatment determined?
What if the injured person needs fewer than the minimum number of visits and is discharged before completing the minimum number of visits?
If the number of sessions delivered is fewer than the minimum number of visits required in the block, we will pay the provider for 50 per cent of the block fee.
If the person is discharged early, i.e., in block one, does the provider need to complete and submit the mid-point report?
No, in this case, the provider does not need to submit a mid-point report. If the person is fully recovered and/or discharged in, or at the end of, block one, submit the care and outcomes summary and clearly indicate the rationale for early discharge. Once we receive the completed care and outcomes summary and the previously submitted initial assessment report, payment for block one will be released.
Can more than one regulated health professional provide treatment under the musculoskeletal program of care?
An interdisciplinary team may deliver the musculoskeletal program of care, but only one regulated health professional completes the report for each of the reporting requirements and submit bills for the services.
Can an injured person change to a different provider after they have started receiving treatments in the musculoskeletal program of care?
An injured person who has begun treatment in the musculoskeletal program of care and wishes to continue treatment with another provider must get approval from the WSIB. The person should call their WSIB case manager or nurse consultant to get approval.
If an injured person has a mild traumatic brain injury/concussion and a musculoskeletal injury, can they receive treatment in both programs of care?
Yes. Care can be delivered through the mild traumatic brain injury program of care at the same time as the musculoskeletal program of care, if the injured person meets the admission criteria for each program.
For example, in instances where the injured person has entitlement to a soft tissue injury (e.g., sprain/strain to the lower extremity) as well as a mild traumatic brain injury, the health care professional could bill both the musculoskeletal and the mild traumatic brain injury program of care.
In cases where the mild traumatic brain injury program of care is delivered, treatment of the neck is included in the mild traumatic brain injury program of care and will not be considered as a single zone of injury within the musculoskeletal program of care.
If the injured person has missed an appointment, do I need to notify the WSIB?
If there is a delay greater than one week due to illness, vacation, etc., call the Clinical Expert Line.
What process do I follow if additional treatment is required?
If the provider expects that the person will need further treatment or services after completing the musculoskeletal program of care, the provider should call the Clinical Expert Line to discuss the claim and evaluate the need for a referral. Our clinical experts can be contacted at 416-344-5739 or toll free 1-866-716-1299 Monday to Friday from 7:30 a.m. to 5 p.m.
The clinical expert may ask for more information about: the type and frequency of treatment provided during the program; the injured person’s response to treatment; description of any persistent barriers; and updated clinical and return-to-work information. Once the clinical expert has reviewed the details of the claim, they will make a recommendation about the request for further treatment.
Can an injured person attend simultaneous treatment with two different providers for the same injury area?
No, this is not allowed. Health care providers should ask the injured person if they are already receiving treatment with another provider, before accepting them for treatment.
Are equipment and devices, such as braces and splints, pre-approved in the musculoskeletal program of care?
No, payment for equipment and devices is not pre-approved when receiving treatment in the new musculoskeletal program of care. If you recommend equipment or devices for an injured person, call the WSIB Nurse Consultant for approval.
Communicating with us
When should I call the WSIB?
You must call the WSIB in the following scenarios:
- At the beginning of block one to confirm entitlement to multiple zones of injury
- At the end of block one to confirm entitlement for a single zone of injury, if unknown
Call the Clinical Expert Line if:
- The person does not meet the admission criteria for the musculoskeletal program of care
- At the end of block one if you identify a lack of progress in functional abilities or more than two barriers to recovery
- The person is not expected to meet their recovery and return-to-work goals one week before completing the second block
- There are delays or interruptions (e.g., illness) in services that last beyond one week
- if the person’s recovery is not progressing as expected at any time during the program to discuss options for specialized assessment/treatment.
Call the Case Manager or Nurse Consultant if:
- Additional treatment is needed after the first supplementary block
- The person’s recovery is not progressing as expected at any time during the program
- You are looking for more information related to return to work or employer accommodations to help with your treatment planning
Billing
Can a regulated health professional bill an injured person directly for treatment provided for a musculoskeletal injury?
The WSIB pays for a person’s health care that is required because of a workplace injury. The regulated health professional cannot bill the injured person directly.
Can a regulated health professional use fee-for-service billing for first line of care musculoskeletal injuries?
No, the musculoskeletal program of care is the mandatory first line of care for injured people who meet the admission criteria or are deemed appropriate for treatment within the program.
Will I be paid for treatment delivered in a claim that is denied?
If you have provided or exceeded the minimum number of visits for a single zone of injury, we will pay you for block one regardless of the status of the registered claim. If you provided less than the minimum number of visits in block one, you will receive 50 per cent of the fee for single injury.
Please call the WSIB to ensure the claim is allowed before starting block two of treatment, as you will not be paid for care delivered in block two of a pending or denied claim.
Does the WSIB require electronic billing?
Yes, regulated health professionals must submit bills electronically for all reports (initial assessment report, mid-point report, care and outcomes summary report, and supplementary report where applicable) and the associated treatment block using TELUS Health.
Submit forms within two business days of assessment/treatment completion date and/or discharge date through our online services.
You need to sign up for our online services or sign into your online services account to submit forms.
See detailed instructions in the billing tip sheet. For further information on electronic billing, please call the TELUS Health Solutions Support Centre at 1-866-240-7492 or visit the TELUS website.
Is there an instance where the regulated health professionals would not receive payment for reports and/or treatment?
If we do not receive a copy of the report/form within 14 business days of the service date (assessment or last treatment date), we will not pay the report fee.
We will not pay for treatment if the report/form(s) for the corresponding block has not been submitted:
- Payment of block one will be withheld until we receive both the initial assessment and mid-point reports.
- Payment of block two will be withheld until we receive the care and outcomes summary report.
- Payment of pre-approved supplementary block will be withheld until we receive the supplementary report.
Are the billing codes for this musculoskeletal program of care different from the old programs of care and non-surgical fracture episode of care?
Billing codes for this musculoskeletal program of care are different. Providers must use new service codes when billing for this program. Refer to the fee schedule and billing tips for additional information.
Are there different billing codes for a single zone of injury versus a multiple zones of injury?
There are single and multiple zone billing categories for the musculoskeletal program of care. You would receive an increased fee for delivering care for multiple zones of injury if there is entitlement in the claim for multiple zones of injury.
Refer to the fee schedule and billing tips for additional information.
Who can I contact for payment-related questions?
Health care providers can call us at 1-800-387-0750 or 416-344-1000 and a representative will help direct you to the right person.
Where can I find more information about the musculoskeletal program of care?
Learn more about the musculoskeletal program of care and other programs of care on our website.
For general questions about the musculoskeletal program of care, please call us at 1-800-387-0750 or 416-344-1000.
Updated: